The cavum septum pellucidum (CSP) represents a unique anatomical structure in the brain, located between the lateral ventricles. While small and typically overlooked, this fluid-filled space plays a crucial role in brain development and neuroanatomical organization. Its presence or absence and size variations hold significant value in neurological and developmental research, often informing clinicians about various brain anomalies and related conditions. The cavum septum pellucidum is frequently discussed in the context of fetal development, brain imaging, and neuropsychiatric studies, offering insights into potential correlations with cognitive and motor function impairments.
Understanding the Cavum Septum Pellucidum
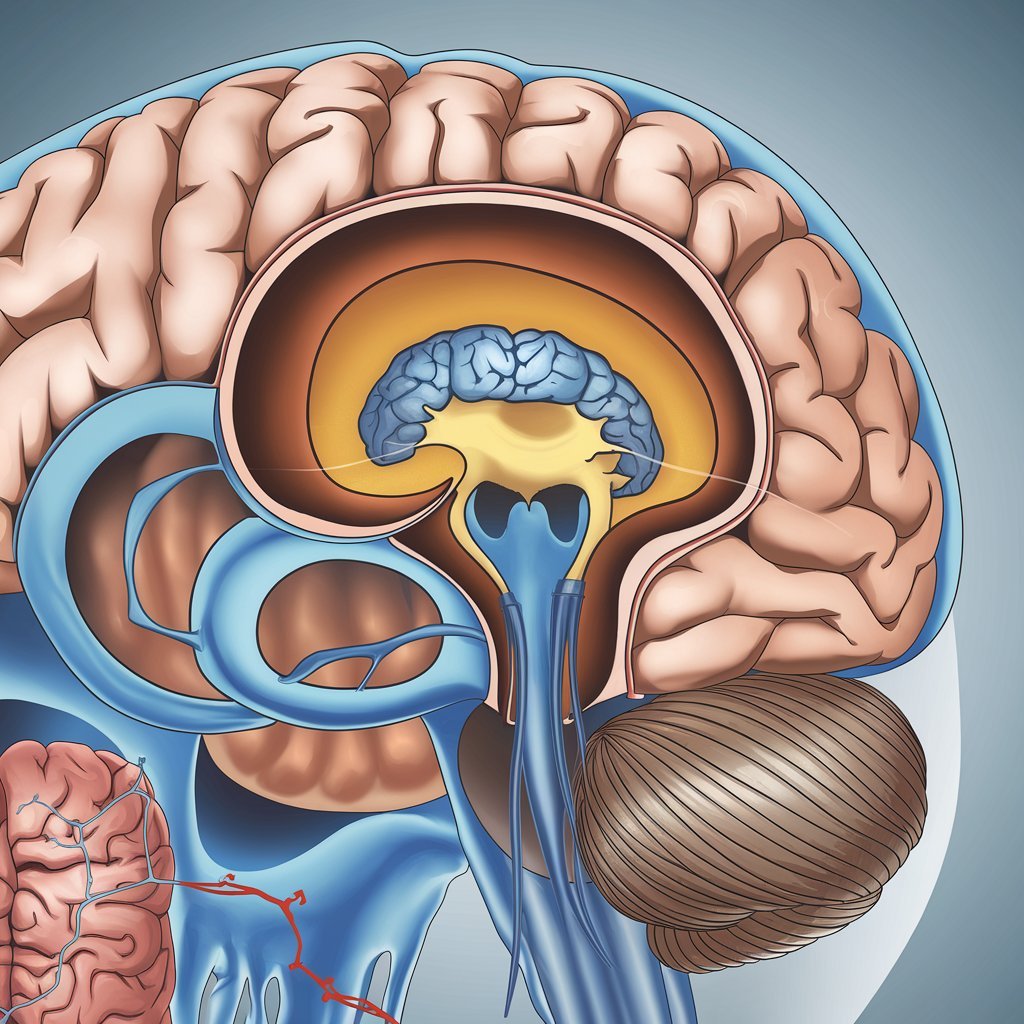
The cavum septum pellucidum is a space found in the midline of the brain, typically situated between two transparent sheets known as the septum pellucidum, which separates the lateral ventricles. This structure becomes evident during fetal brain development and is normally present at birth. Its persistence, however, varies among individuals, with some experiencing a lifelong presence of the cavum, while others see it close as early as infancy.
The role of the cavum septum pellucidum has intrigued neuroscientists, as this unique formation is believed to contribute to a well-organized neural development. Additionally, its relationship with other brain structures and overall brain health is currently under active study.
Formation and Development of the CSP
The cavum septum pellucidum forms during the second trimester of fetal development, commonly between the 12th and 20th weeks of gestation. During this time, the brain undergoes significant morphological changes, and the septum pellucidum’s two transparent membranes begin to develop. These layers are separated by the cavum, a space filled with cerebrospinal fluid (CSF), which serves as a buffer between the developing brain structures.
Normally, the cavum septum pellucidum decreases in size or closes entirely by the time of birth or during the early stages of childhood. However, in certain individuals, this process does not occur, resulting in a condition termed a persistent cavum septum pellucidum. Although often asymptomatic, a persistent CSP is occasionally associated with neurodevelopmental anomalies, which can impact the individual’s cognitive and motor abilities.
Functions of the CSP
Despite its small size, the cavum septum pellucidum holds functional significance in the structural organization of the brain. While traditionally thought to be a vestigial remnant, it is now believed to play a role in neurodevelopment. Its presence helps provide an organized architecture during brain maturation, acting as a reference point for other developing structures in the medial forebrain.
Additionally, the CSP may serve as a protective buffer for nearby brain regions. The fluid within the cavum septum pellucidum is part of the cerebrospinal fluid system, which cushions the brain and spinal cord, possibly providing localized support and protection to the nearby septal nuclei, which are involved in emotional and motivational regulation.
Clinical Significance of CSP
The cavum septum pellucidum has been linked to various clinical conditions, including neurodevelopmental and psychiatric disorders. While a persistent CSP is often benign, its presence has been associated with conditions such as schizophrenia, post-traumatic stress disorder (PTSD), and major depressive disorder. In these cases, CSP persistence may suggest developmental disruptions affecting neural connections within the limbic system.
Moreover, the presence of CSP in adult brains has been noted in individuals who have experienced traumatic brain injury (TBI). Studies suggest that an enlarged CSP may result from brain injury, reflecting tissue damage or neural pathway changes due to trauma. This finding has spurred further investigation into the potential diagnostic and prognostic value of observing CSP size and morphology in brain imaging studies.
Cavum Septum Pellucidum in Fetal Development
The cavum septum pellucidum is commonly examined during routine fetal ultrasound screenings as part of the neuroanatomical assessment. Its presence, size, and position are typically monitored to rule out anomalies that may indicate broader developmental issues. The absence of CSP in a fetus may prompt further testing, as it is often associated with corpus callosum agenesis—a developmental disorder involving the brain’s main interhemispheric communication structure.
Cavum Septum Pellucidum in Neonatal Imaging
In newborns, the cavum septum pellucidum is often examined through neonatal brain imaging, particularly in cases of premature birth or other risk factors for developmental complications. Neonatologists may assess the cavum’s characteristics to identify any potential risks for neurodevelopmental disorders.
While the absence or small size of CSP at birth may not immediately suggest an issue, abnormal sizes or configurations have been linked to various conditions, including genetic disorders and structural brain anomalies. Therefore, detailed imaging and follow-up assessments are generally conducted in such cases to monitor brain development.
Diagnostic Imaging and the Cavum Septum Pellucidum
Modern imaging techniques such as MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) scans have greatly improved the ability to study the cavum septum pellucidum in detail. MRI, in particular, provides high-resolution images of the brain, allowing clinicians to examine the CSP’s structure, size, and any potential anomalies closely.
In clinical practice, MRI is frequently used to assess CSP size in patients with neuropsychiatric symptoms. When an unusually large or persistent CSP is detected, further neurological evaluations may be considered to explore any underlying conditions.
The Role of CSP in Neuropsychiatric Research
Research has shown a correlation between the cavum septum pellucidum and certain psychiatric conditions, particularly schizophrenia and bipolar disorder. Studies indicate that an abnormally large CSP is more frequently observed in individuals with these disorders compared to the general population.
The underlying mechanisms of this association remain under investigation. However, it is hypothesized that the abnormal persistence of CSP may reflect disruptions in the formation of brain networks critical for emotional regulation and cognitive processing. By studying the CSP, researchers hope to uncover insights into the developmental origins of these conditions and improve early diagnostic practices.
Cavum Septum Pellucidum and Trauma
In trauma-related research, the cavum septum pellucidum has been studied extensively due to its prevalence in individuals with a history of traumatic brain injury (TBI). An enlarged CSP has been identified as a marker of head trauma, particularly in athletes exposed to repeated concussions and military personnel who have experienced blast injuries.
The observation of CSP enlargement in these populations suggests a possible connection between trauma-induced changes in brain morphology and long-term cognitive and emotional effects. Consequently, CSP assessment is considered a useful tool for clinicians managing individuals with a history of trauma or concussion.
Genetic Factors Influencing Cavum Septum Pellucidum Development
Genetics plays a significant role in the development and persistence of the cavum septum pellucidum. Some genetic syndromes, such as septo-optic dysplasia, often involve anomalies in CSP formation, alongside other neuroanatomical abnormalities. Variants in specific genes related to brain development can influence the formation, size, and closure rate of the cavum, underscoring the importance of genetic factors in CSP morphology.
Treatment and Management Approaches
Since the cavum septum pellucidum is typically asymptomatic, treatment is rarely required. In cases where CSP persistence is accompanied by symptoms, the primary approach involves addressing the underlying neurological or psychiatric condition. For example, neuropsychiatric interventions may be considered for individuals with CSP-associated psychiatric symptoms, while patients with trauma-related CSP enlargement may receive treatment focused on cognitive rehabilitation and symptomatic relief.
Future Directions in Cavum Septum Pellucidum Research
As neuroimaging technology advances, a deeper understanding of the cavum septum pellucidum and its clinical implications is expected to emerge. Researchers are exploring CSP’s potential as a biomarker for early detection of neurodevelopmental and neuropsychiatric disorders. Future studies are likely to provide further insights into the role of CSP in brain connectivity and function, advancing the field of neurodevelopmental research and mental health diagnostics.
FAQs
What is the CSP?
The CSP is a fluid-filled cavity situated between the lateral ventricles in the brain, often present during fetal development and sometimes persisting into adulthood.
Does the CSP have a function?
It primarily contributes to neurodevelopment and provides structural organization, though it is often considered a vestigial space in adults.
What does a large CSP indicate?
A large CSP may be associated with conditions such as schizophrenia, PTSD, and traumatic brain injury, although it can also be asymptomatic.
Is a persistent CSP harmful?
Typically, no. Many individuals with a persistent CSP experience no symptoms. However, it may correlate with certain neurological or psychiatric conditions.
How is CSP identified?
Imaging techniques, primarily MRI, are used to visualize and assess CSP size, structure, and potential anomalies in clinical settings.
Can CSP close on its own?
Yes, CSP typically closes after birth or during early childhood, although it may remain open in some individuals without causing symptoms.
Are there any treatments for an enlarged CSP?
Treatment usually focuses on managing symptoms of associated conditions, if any, rather than addressing CSP itself.